In 2006, I was 15 in the semester-long health class mandated by my public high school. Most of what I remember learning about STIs was “STIs are bad – don’t get them – use condoms”. I really don’t remember learning much about HPV specifically at all.
Now as a non-monogamous woman in her early 30s, I believe that being proactive about my sexual health is of the utmost importance. Like the majority of the ENM population I know, I have the safest sex I can by:
- getting tested regularly
- communicating with potential partners about their STI status
- using barriers until trust and regularity is built
To me, there was no possible way I could get an STI – I was doing everything right.
On May 14, 2021 I received a call from my gynecologist letting me know that my pap smear tested positive for HPV.
My heart stopped. I knew nothing about HPV except that “it leads to cervical cancer”. I was ashamed, I was speechless, I was in utter shock. How did this happen and what did it mean for my life going forward?
Trying to alleviate my fears over the phone, my doctor told me that HPV is so common that they consider it the “common cold” of STIs. As you can probably imagine, that didn’t ease my mind. We scheduled a procedure called a colposcopy and she said we’d take it from there.
Common HPV Myths
- Once you test positive, you’ll have it forever
- HPV is only transmitted sexually
- HPV cannot be transmitted if using condoms
- If you test positive for HPV it means your partner cheated on you (typical monogamous myth)
- There’s no way to prevent HPV
- If you have HPV, it will absolutely turn into cervical cancer
- Only women need to worry about HPV
If you’ve ever believed one or more of the above statements, read on; and don’t worry – you’re in the majority.
The STI Stigma
As soon as I got off the phone I dove into research. My mind was spinning – being non-monogamous, would anyone ever want me again? I called my two current partners, and thankfully they were both highly supportive.
Prior to testing positive for HPV and actually doing research – I have a feeling that if any potential partners would have disclosed to me that they ever had HPV, I would not have pursued a relationship. I’m part of the problem. We, as a society, have such a negative view on STIs/STDs that we don’t want to associate with anyone known to have them. The moment we find out someone’s positive status, rather than taking time to learn about it, we put up a wall and move on to the next person. We view STI positive folks as unclean, and we make assumptions that they probably engage in risky sex, because that’s what public education sex-ed taught us.
In the time since I received my positive result, I have been a big advocate for talking about HPV with potential partners and people I chat with on dating sites, with the goal of education and destigmatization. When I open up about my past positive HPV result, I’ve had people say “oh, did you not use a condom?”, “didn’t you have signs or symptoms?”, “how could you not know who you got it from??” The fact that these responses have been the vast majority shows me that there is a dire need for better HPV education.
“I felt like it was my fault, that I had done something wrong, because I had HPV … It’s sexually transmitted so there was always this sense that it was somehow my doing and that I could have avoided this … It seems that relatively little has changed in regards to HPV – the level of knowledge, how it is viewed, and how it is spoken about. I feel saddened that there are still so many women and people with a cervix, finding out they have HPV, feeling terrified about their future and possibly blaming themselves.”
Jess Phillips (Shearing, 2021)
In a survey conducted by one of the UK’s leading cancer charities, they found that only 22% of women polled would date someone with HPV1
I can tell you that when I tested positive for HPV, I hadn’t had barrier-less “unsafe” sex. My sexual partners were all “STI negative” based on their most recent tests. So how did this happen?
Human Papillomavirus
STI or STD?
I see so many people using STI and STD interchangeably, but as I recently learned from a Multiamory episode, an STI is an infection and an STD is a disease. Duh, we all know the acronyms, but what makes them different?
Having an STI means that your body has been infected with something (bacteria, parasite) that hasn’t yet developed into a disease. Sometimes infections clear up on their own, and sometimes they can develop into STDs – which are diseases that affect your body negatively and produce signs and symptoms.2 If we think of it outside of sex, a person can have an e. coli infection (infection) from contaminated food – that causes food poisoning (disease). In the world of STIs/STDs, HPV is an STI that can turn into genital warts or cervical cancer – both STDs.
So, HPV is an infection. Got it.
Because HPV is an infection, there are no signs or symptoms. This means, that it can be transmitted between partners and you could have no idea. As an infection, in most cases your body is able to fight it off and it goes away on its own.
Men cannot get tested for HPV.
Let me say that again, at present, humans without a cervix cannot get tested for HPV because to test for HPV, a swab of the cervix is needed. Prior to digging into HPV research, I had no idea that this was only something humans with cervixes could test for. I heard my potential male partners say they were “negative for everything” upon receiving screening results and assumed it literally meant everything. They may have been “negative for everything” included in the screening their doctor ordered, but that screening did not and could not include HPV.
There are over 150 strains of HPV but we only test for a portion of them.
Researchers have identified which of the 150+ strains are considered high-risk, and which are considered low-risk. There are 14 strains classified as high-risk that have been linked to causing cell mutations and can lead to various cancers. These high-risk strains are: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68; with 16 and 18 responsible for the majority of HPV related cancer. Low-risk strains include 6, 11, 42, 43, and 44; with 6 and 11 causing 90% of genital warts.
When cervix owners get tested for HPV, they are getting tested for any of the above mentioned strains. This means that the remaining ~130+ strains come and go without detection.
A person can test positive for one or more of the high-risk strains and it doesn’t mean it will develop into cancer. It just means that the presence of those strains could lead to cancer, because of certain genes present within those virus strains.
With how prevalent it is, I’ve seen statistics estimating that 80% of sexually active adults will be infected with HPV at one point or another, but most will never realize they have it. Because half the population can’t get tested, and because it often comes and goes without detection, there isn’t a way to pinpoint the exact statistic, but scientists can infer based on the number of new positive results each year.
“HPV is the most common STD, but most of the time it isn’t a big deal. It usually goes away on its own, and most people don’t even know that they ever had HPV. Remember that most people who have sex get HPV at some point in their lives. You don’t need to be ashamed or afraid.”
Planned Parenthood3
The point I’m trying to make is that getting a positive HPV result is not the end of the world – in fact – it’s extremely common. While most strains are nothing to worry about, when high-risk strains are left untreated, they have the potential to cause cancer.
HPV and Cancer
We mainly think about cervical cancer because virtually all cervical cancers are caused by HPV, however other cancers can be caused by HPV too:
- Oropharyngeal Cancer (type of throat cancer – generally in tonsils or back of tongue)
- 70% of these cancers are caused by HPV
- Anal Cancer
- 90% of these cancers are caused by HPV
- Penile Cancer
- 60% of these cancers are caused by HPV
- Vaginal Cancer
- 75% of these cancers are caused by HPV
- Vulvar Cancer
- 70% of these cancers are caused by HPV4
I know 3 different men in their 60s who had HPV-related oropharyngeal cancer within the past 10 years. I’ve met some individuals with the belief that “HPV causes cervical cancer – I’m a man – I’m not at risk” and that’s simply not true. HPV affects all genders.
High-risk HPV is easily treatable before it develops into cancer which is why regular testing and early detection is crucial.
Transmission and Detection
Fun fact – not all types of HPV are sexually transmitted (if you’ve ever had a common wart on your hands or a plantar wart on your feet – you’ve had HPV!), but in this blog, I’m focusing on the strains of HPV considered to be an STIs. HPV is spread via skin to skin contact so while barriers may add slightly more protection, they don’t protect users fully. HPV is spread when genitals (vulva, vagina, cervix, penis, anus) touch someone else’s genitals, mouth, or throat either directly or indirectly (hands going from one person’s genitals to another’s). HPV can be transmitted even without intercourse (oral, vaginal, anal).3
By high school sex-ed’s logic, a person can be doing everything “right” and still contract HPV. Hence why as of late, I’ve subscribed to the logic that there is actually no way to have “safe sex” – meaning sex can never be 100% safe. Armed with knowledge of transmission, we can use regular STI screenings and barriers as ways to have “safer sex”.
HPV tests are not part of a typical “STI screening”. In order to test for HPV, a small sample of cervical cells need to be collected. Typically, this is done at the same time as a pap smear, but it isn’t always guaranteed so be sure to talk to your doctor when getting your pap smear. A pap smear tests for cervical cell abnormalities and an HPV test detects if any high-risk HPV strains are present within the sample.
Currently, the American Cancer Society recommends that cervix owners age 25-65 get a combined pap smear/HPV test every 5 years. The reasoning for the gap between tests comes from understanding that a positive HPV result causes unnecessary alarm, often clears up on its own, and doesn’t typically evolve into cancer.
“Although HPV infection of the cervix is very common, most infections will be controlled by the immune system over the course of 1 to 2 years. Because most HPV infections are transient and produce only temporary changes in cervical cells, overly frequent screening could detect HPV infections or cell changes that would never cause cancer. Treating abnormalities that would have gone away on their own can cause needless psychological stress. Follow-up tests and treatments can also be uncomfortable, and the removal of cervical tissue has the potential to weaken the cervix and may affect fertility or slightly increase the rate of premature delivery, depending on how much tissue is removed.”
National Cancer Institute5
Being non-monogamous, and having had a positive result for a high-risk strain in the past, I’m currently opting to get this done yearly at the recommendation of my doctor in order to monitor things and make sure that it doesn’t stick around to turn into cancer.
Tracking HPV Transmission is Virtually Impossible.
The first question people always want to know when they test positive for an STI is – where did this come from? Unfortunately this is extremely hard to track for HPV. For starters, half the population can’t get tested, so you can’t just go to your male partners and say “okay, everyone go get tested!” like you can with other STIs.
Additionally, (and this is where monogamous folks always worry about cheating) it’s possible that the HPV infection has been dormant in your body for years before emerging to produce a positive result. I tested positive for HPV in 5/2021. I’ve been sexually active since 2007, and it’s entirely possible I could have gotten it from any of my lifetime sex partners and it was just laying dormant until now. This is similar to how the chickenpox virus can lay dormant for years and then reemerge as shingles later in life. If you’re in a monogamous relationship and you or your partner all of a sudden test positive for HPV, one of you likely contracted it from a prior partner long before your current relationship.
HPV Prevention
A positive HPV result shouldn’t be scary, as it most often clears up on its own. However, because high-risk strains can develop into life-threatening cancers, we have reason to want to prevent HPV in whatever way we can.
Currently, the only way available to prevent against certain strains of HPV is the HPV vaccine.
Nowadays, most adolescents, both boys and girls, should hopefully be getting Gardasil 9 as recommended by their doctors. However, I’m assuming most of my readers are in a similar age group as myself, who didn’t have the vaccine available in early adolescence.
The original Gardasil vaccine came out in 2006 (I was 16) and protected against 4 strains of HPV: 6, 11, 16, and 18. Remembering from a few paragraphs ago, this includes the two low-risk strains that make up the majority of genital warts, and the two high-risk strains that cause the most cervical cancer. I ended up getting this vaccine in 2010 of my own choice even though at the time doctors thought there was no benefit once an individual was sexually active.
*This belief came about from knowing how prevalent HPV is, under the assumption that all sexually active adults are going to get HPV regardless. It was an assumption that once HPV was contracted the vaccine provided no protection. However, even if you were positive for one of the 4 strains, it would still provide protection against the other 3 you didn’t already contract*
Gardasil 9 came out in 2014 and protects against 9 strains of HPV: 6, 11, 16, 18, 31, 33, 45, 52, and 58. It adds protection against 5 other high-risk strains that the original Gardasil vaccine didn’t cover. It’s a three-shot series and once fully vaccinated, the individual is immune to those 9 HPV strains. They can’t contract them, they can’t spread them.
Men can’t get tested for HPV, but they can get the HPV vaccine to eliminate the possibility of contracting and transmitting 7 high-risk and 2 low-risk strains. Not only does this cut down on the likelihood that they will spread cancer-causing strains to partners, but it cuts down on the likelihood that they’ll contract cancer-causing strains themselves.
To my knowledge, most insurance policies cover Gardasil 9 100% until age 45, even if you already had the original, 4-strain Gardasil. Being non-monogamous and realizing I have increased risk of coming in contact with HPV, I’d been asking both my PCP and my gynecologist for Gardasil 9 from the moment I verified that it would be 100% covered by my insurance. Both were opposed because they assumed that it wouldn’t give me any additional protection – that I was already a lost cause since I was in my 30s and sexually active with multiple partners. At the time, not knowing what I do now about HPV, I accepted that answer from them and stopped asking. My gynecologist even told me that she was pretty sure my insurance wouldn’t cover it since I already had the original Gardasil vaccine – even though I had called my insurance company directly to verify and they confirmed that Gardasil 9 would be covered for me. The day my gynecologist called to let me know about my positive HPV result, she said she would finally sign off on approval for my Gardasil 9 vaccine if I still wanted it. I’m relieved to say that my third and final dose was 11/2021. I’m now protected against any of the strains I didn’t already have.
So You’re Positive For HPV. Now What?
First things first, breathe and remember that you are in the majority.
Deciphering Results
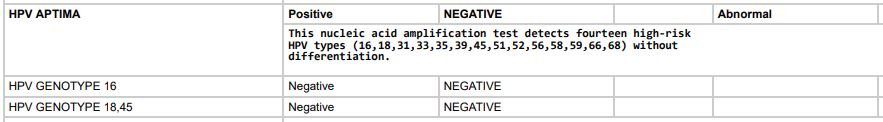
A positive HPV result means that one or more high-risk strains were detected in your cervical cells. All labs are different and as such the information given to you may vary. When my doctor called, I was told that although my pap was normal, it was HPV positive. Typically, normal paps that are HPV positive simply mean that you have a current HPV infection but it hasn’t affected your cervical cells and is believed that it will pass on it’s own. However, being non-monogamous classifies me as “high-risk” and since I’d received an abnormal but HPV negative screening in the past, my doctor wanted to schedule a colposcopy (which is a fancy way to say “more in depth examination of your cervix”). Colposcopies are typically recommended for pap smears with high-grade abnormalities, and/or HPV positive tests that also are positive for genotypes 16 or 18. I had no abnormalities present, but was positive for “high-risk HPV”. My test further detailed that they screened for genotypes 16, 18, and 45 and I was negative for all three.
Abnormal pap results are broken down into which type of abnormalities were detected, based on severity and how precancerous they are.
- Low-Grade abnormalities
- ASC-US
- LSIL
- ASC-H
- High-Grade abnormalities
- HSIL
- AGC
Now – I’m going to get a little technical; bear with me – I’m a biology nerd. If you aren’t interested in the science behind HPV testing, feel free to skip to the next paragraph.
HPV positive results may be presented in different ways, based on the different testing methods available. The HPV Aptima (AHPV) test is currently the most accurate at detecting active HPV infections caused by the 14 high-risk strains. Prior to AHPV testing, the gold standard was HC2 testing. HC2 testing looks for the presence of HPV DNA from the 14 strains, and while it’s helps determine if HPV was ever present, the presence of DNA alone doesn’t indicate if the virus is active or not. DNA could have been residually present from infections that were fought off, and as such, poses no risk of causing cancer (this test leads to higher false positives.) The AHPV test detects mRNA from the 14 strains. Presence of mRNA indicates that the HPV infection is likely active because the virus is replicating. Specifically, AHPV looks for oncoproteins E6 and E7 within the mRNA, which are known to degrade tumor-suppressor proteins leading to the possible generation of tumors/cancer. When we test for HPV, we do so because we are trying to prevent the cancer it could turn into; if it isn’t causing cancer, it isn’t harming us so we don’t really care about it. A positive AHPV result tells you that mRNA containing E6/E7 was present in your cervical cell sample. Once a positive result occurs, they can test more specifically to determine if the genotype of the HPV strain present is 16 or 18. (6,7)
Remember that even if you get results that indicate high-grade abnormalities, or are positive for HPV strains 16 or 18, it does not mean that you have cancer.
Depending on your pap results and HPV stain results, your doctor will determine if they need to do a colposcopy or if you should just get re-tested again in a year. If they recommend re-testing in a year, you can be assured that your doctor believes that it’s likely your HPV will clear up on its own without progressing to cancer.
Colposcopy
If a colposcopy is recommended, you will schedule the procedure for the near future. During your appointment, your doctor will spray a special solution onto your cervix as you’re laying down. This solution makes abnormal cells easier to spot by turning them white. Then, your doctor will look through a colposcope which enlarges the view of your cervical cells to better analyze the abnormal cells. The colposcope uses technology to determine if any of the abnormalities may be cancerous – if they are, then your doctor will take a biopsy of each area in question. To me, the biopsy wasn’t painful. My doctor sprayed a numbing spray and removed 3 small sections of my cervix. They apply a coagulant to prevent bleeding, but recommend using a pad immediately after just in case. I barely experienced any bleeding and the only discomfort I had was mild cramps later that evening.
A few days later, once testing of your cervix samples is complete, you will receive your results which can be any of the following:
- Normal
- no abnormal cells detected
- no treatment necessary
- CIN1
- low grade abnormalities on the surface or up to 1/3 deep into the outer cervix
- no treatment recommended because CIN1 cells typically revert back to normal on their own
- CIN2
- high grade abnormalities up to 2/3 deep into the outer cervix
- treatment options vary – can either be monitored or treated
- CIN3
- high grade abnormalities in the full depth of the outer cervix
- treatment recommended
- Treatment options include LEEP (loop electrosurgical excision procedure) and cone biopsies to remove all of the precancerous abnormalities. LEEP is the preferred method due to higher complications associated with cone biopsies
My results came back CIN1, meaning that no further action was needed. CIN1 cells most often heal themselves on their own, so there is no cause for me to worry. I’ll get retested this year to see whether or not my body fought off the HPV.
You Are Not Alone
When I received my positive result, I was devastated. I didn’t want to talk to anyone because I was so ashamed. I felt so alone. One day, I broke down and confided in my closest group of friends, who also happen to be ENM. To my surprise, I discovered that several of them had received positive HPV results in their lifetime, yet they were all living happy, non-monogamous lives free from discrimination. One had a similar experience to me, and one had to go through the LEEP treatment but in the end, they were both HPV negative. Just knowing two other people who had been “HPV positive” helped crush the stigma for me. I try to be more open about it in my daily life, promoting Gardasil 9 to whoever I can, and as a result, several other friends of mine have reached out to share their experiences with HPV.
In May of 2021, I thought I was the only person I knew with HPV. Today in January of 2022, I personally know 15 other close women in my life who were or currently are HPV positive. All 16 of us felt alone and ashamed. All 16 of us were terrified of the stigma associated with STIs and specifically HPV. All 16 of us endured intense psychological stress from not realizing how “minor” HPV really is. With how prevalent this infection is, it needs to be talked about more than it is.
If you’re someone who is currently HPV positive, my best advice is to learn all that you can so you can help educate those who stigmatize it. If you are in a relationship with someone who is HPV positive, give them all your support. You probably have it too even though you may not be able to get tested. If you are considering dating someone who is HPV positive, don’t let that stop you from having a sexual relationship with them. Odds are that if you’re sexually active you’ve had one or more strains already. HPV isn’t the bad guy, cancer is.
If you are sexually active and you haven’t received the Gardasil 9 vaccine, please get it. Even if you’re monogamous. Even if you don’t have a cervix. Even if you’ve been positive for HPV in the past. Protect yourself and protect others.
Comment below with one new piece of information you learned today!
References:
- Shearing, H. (2021, June 13). Jess Phillips: Ditch HPV stigma to avoid the shame I felt. BBC News. Retrieved January 26, 2022, from https://www.bbc.com/news/uk-57438881 ↩
- Lindgren, J., Matlack, E., & Winston, D. (Hosts). (2021, December 7). Safer Sex Part 1 (No. 351) [Audio podcast episode]. In Multiamory. Multiamory LLC. https://www.multiamory.com/podcast/351-safer-sex-part-1 ↩
- What Is HPV & How Do You Get It? Planned Parenthood. (n.d.). Retrieved January 25, 2022, from https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/hpv ↩
- HPV and Cancer. National Cancer Institute. (2021, October 25). Retrieved January 25, 2022, from https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer ↩
- HPV and Pap Testing. National Cancer Institute. (2019, December 20). Retrieved January 25, 2022, from https://www.cancer.gov/types/cervical/pap-hpv-testing-fact-sheet ↩
- Thomas, J. T., & Laimins, L. A. (1998). Human papillomavirus oncoproteins E6 and E7 independently abrogate the mitotic spindle checkpoint. Journal of Virology, 72(2), 1131–1137. https://doi.org/10.1128/jvi.72.2.1131-1137.1998 ↩
- Yim, E.-K., & Park, J.-S. (2005). The role of HPV E6 and E7 oncoproteins in HPV-associated cervical carcinogenesis. Cancer Research and Treatment, 37(6), 319–324. https://doi.org/10.4143/crt.2005.37.6.319 ↩
Your post helps reduce the stigma associated with HPV for both females and males. It appears to be a treatable infection if caught early. Those who get the STI shouldn’t “suffer in silence”. Hopefully they’ll inform their partners.
LikeLiked by 1 person
Thank you so much for reading! When I shared this to my social media accounts, 100% of my friends who interacted with the post were women. I think that illustrates how a lot of men just shrug it off thinking it’s a “women’s disease”, so it means a lot that you too the time to read this one!
LikeLiked by 1 person
most guys (including Dr.s) don’t believe they can’t catch HPV b/c they don’t have symptoms. If they do a lot of oral, they may see wartsin their mouth and on their tongue. Dr.’s will assume it’s some kind of herpes & incurable.
LikeLiked by 1 person
Exactly. Until it develops into throat cancer YEARS down the road. As I mentioned in the post – I personally know three men in their 60s who got throat cancer and when the tumors were biopsied – it was HPV. Throat cancer is a BIG deal. I wish we could get the word out to more men so they realize they aren’t unaffected.
LikeLiked by 1 person
Thank you for this post… I was recently diagnosed with high-grade HPV and had to have a LEEP procedure, which my doctor assured me was successful and that the cells she removed, which she tested, showed to be all of the pre-cancerous cells that had been present. I’ve been beating myself up, at 40 I should have known better and been safer sexually but I knew I was being monogamous and even though I trust that my partner was too, he could’ve been living with HPV for awhile now and not known it. I also received the Guardisil vaccination but I’ve been very depressed lately and questioning all of my life decisions. 🙁 Your post has helped… Thank you…
LikeLiked by 1 person
I’m so glad my post helped! I know how easy it is to fall into that rabbit-hole of beating yourself up. I have no doubt that you were doing everything right. We just don’t get enough education on HPV and it’s SO stigmatized that people don’t talk about it enough – as common as it is. Easier said than done, but try not to let this get you down. You have no reason to question your life decisions. You did nothing wrong. Sending you my positive vibes so that you can heal from your LEEP and this whole mental experience. Thank you for sharing your story and know you’re not alone!
LikeLiked by 1 person
Pingback: HPV-iversary | The Polyamorous Millennial
Pingback: Part of the 90%: 2023 HPV Update | The Polyamorous Millennial
Pingback: #AMA (Ask Me Anything) Responses | The Polyamorous Millennial